Improving every aspect of the healthcare experience.
By combining virtual care, clinician-led navigation, and patient advocacy in one seamless solution, we deliver higher-quality care for millions of employees and more savings for employers.

Delivering outsized results for leading employers
Healthcare solutions designed for healthier employees
Learn more about why top employers choose us.

Included Health Introduces Next Frontier of Virtual Care: The Specialty Care Clinic.
Healthcare that works better for everyone

A uniquely member-first experience
When members feel like they’re the first priority, they’re more likely to get the care they need. That’s why our members come to us for one thing and end up returning for more and more support.
4.9/5
member rating
60%
of our members are repeat users within the first six months
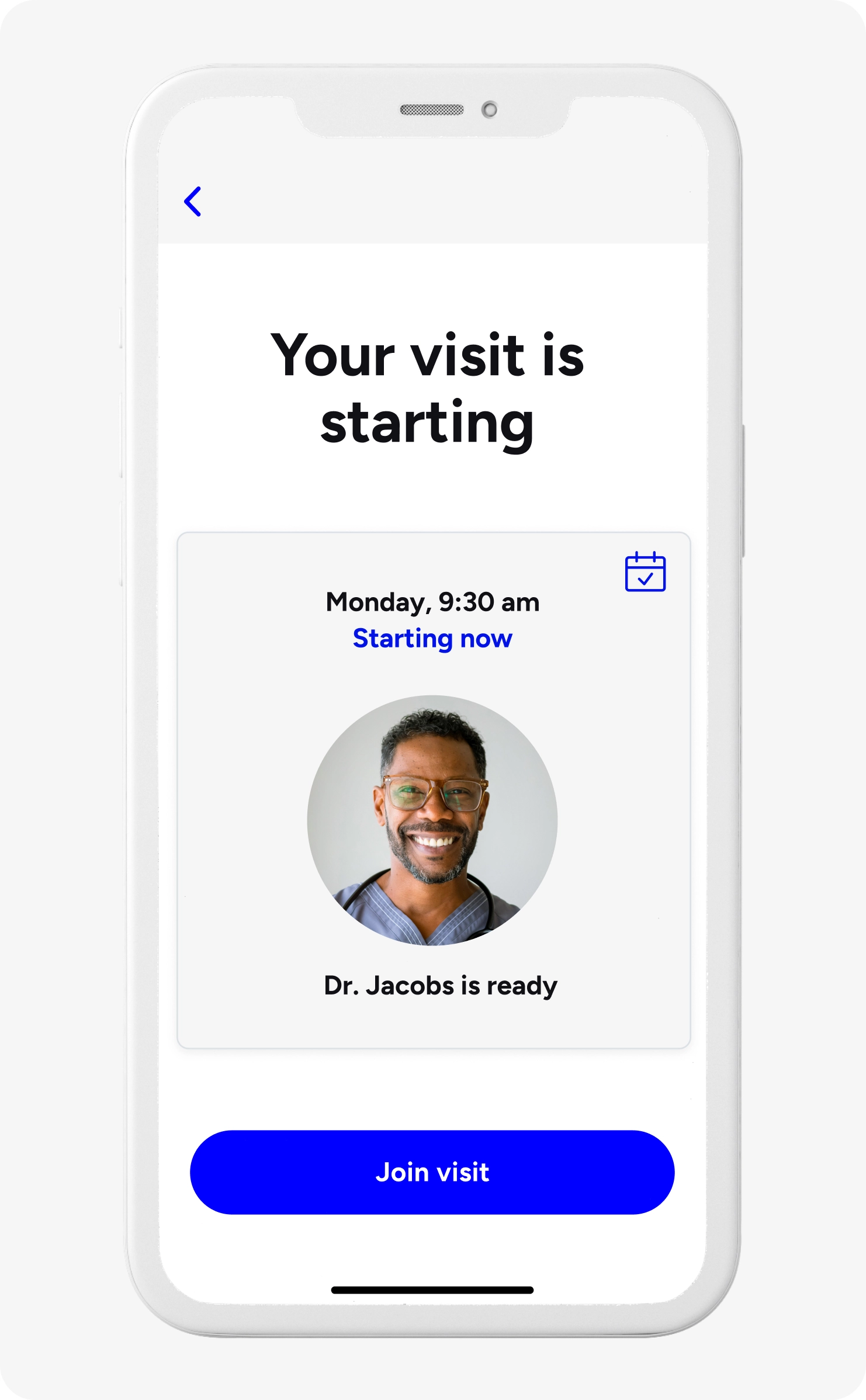
Navigation and care connected by a single experience
Our solutions seamlessly integrate with your overall benefits strategy to provide better care for every need—physical to mental, preventive to chronic, administrative to clinical.
65%
of our doctor’s visits started with a member’s benefit question
>50+%
of our members use more than one service

Data that identifies and anticipates needs
With real-time, multi-source data and in-house predictive algorithms, we segment our population based on need to engage at scale, reaching those who need care now and directing those at risk to better preventive care.
74%
high-cost, high-needs households engaged
91%
more members connected with high-quality providers
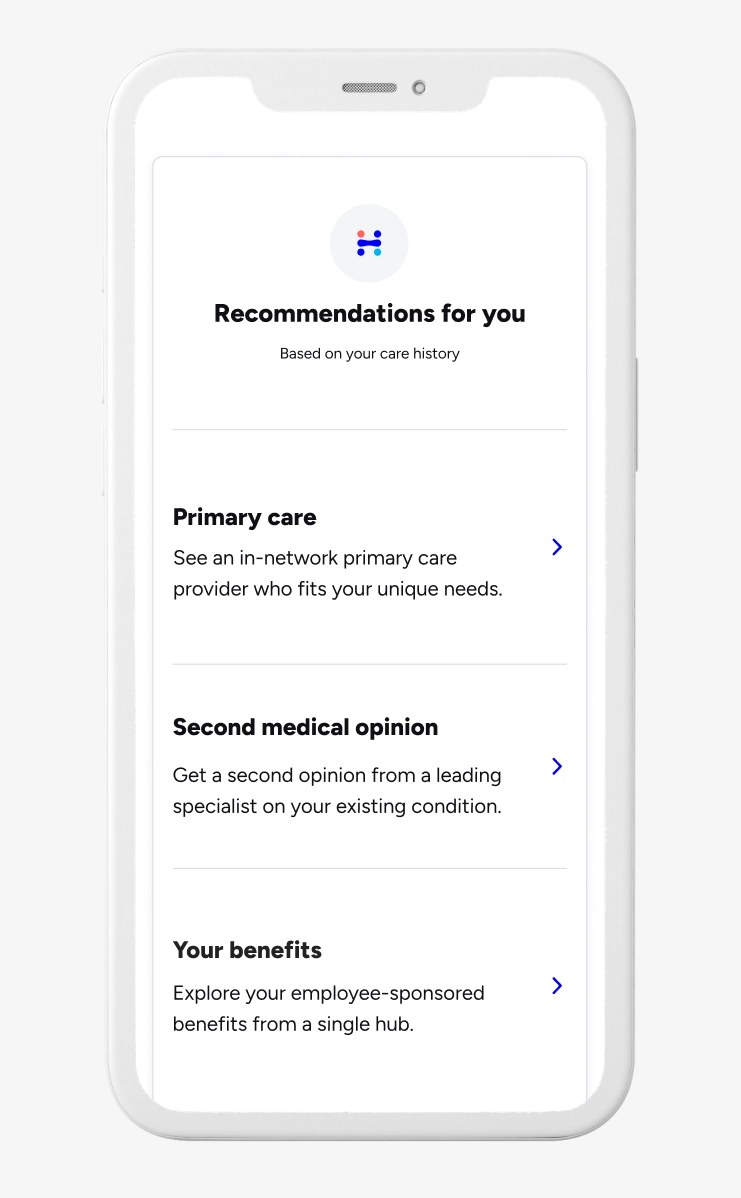
Clinical expertise drives better outcomes
Our clinical staff do more than treat members: They guide our entire solution, providing insights on the digital experience, the standards we aim for, and the care we deliver to millions.
$325M
annual savings from high-quality referrals
66%
of members change their treatment after a second opinion