
As we navigate the complex terrain of 21st-century healthcare, it becomes increasingly clear that traditional approaches to care are giving way to innovative solutions that leverage the power of virtual primary care (VPC). However, there are lingering myths surrounding the impact and efficacy of VPC that need to be addressed.
Myth #1:
Virtual primary care is “just another expense”
One potential barrier to implementing integrated virtual primary care is the belief that it is an additive service that simply adds to overall healthcare costs.
Reality #1:
VPC generates cost savings by reducing expensive in-person visits
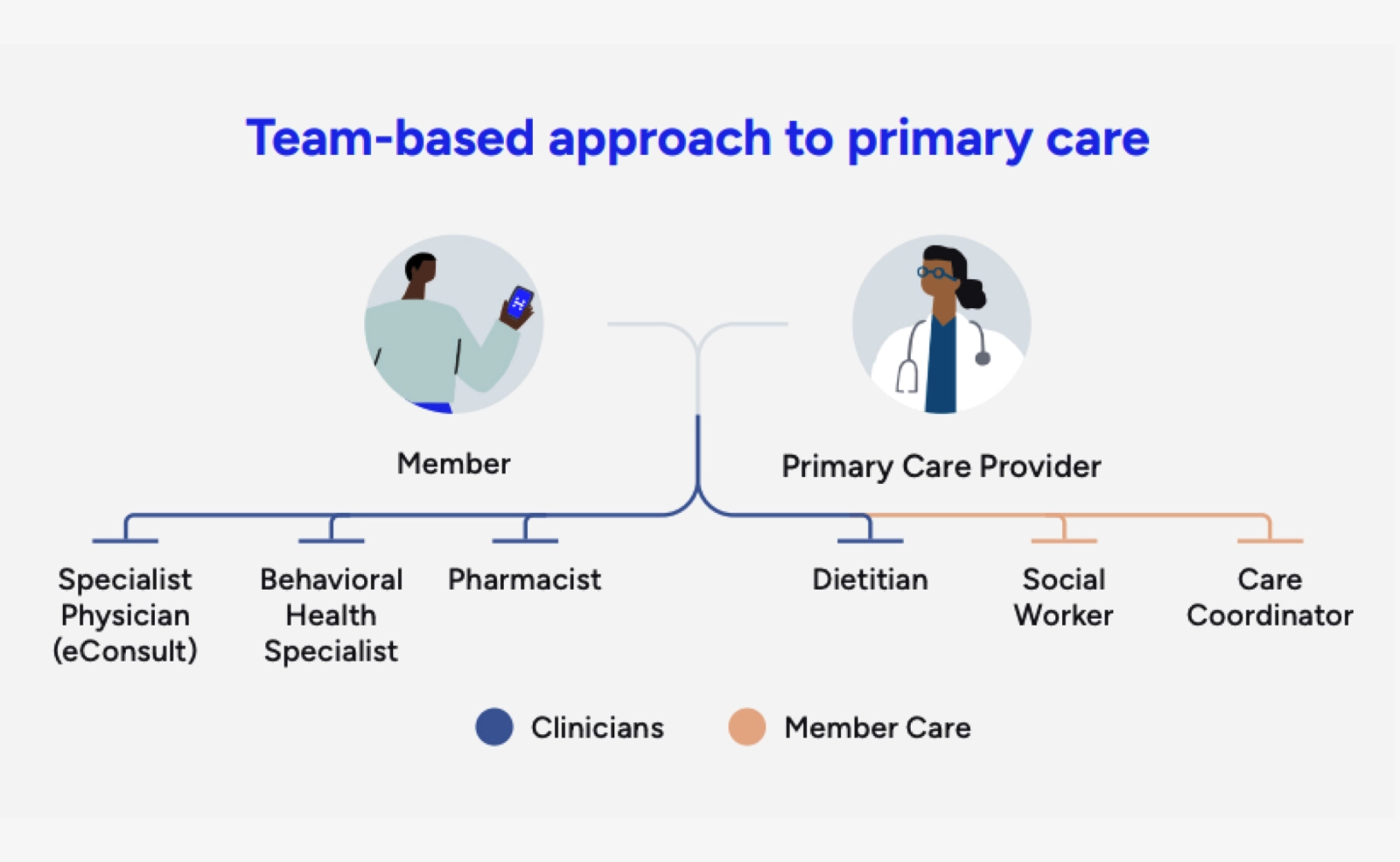
Virtual primary care, encompassing primary care, behavioral health, and urgent care, generates replacement savings by diverting individuals from more expensive in-person visits, including trips to the emergency department. When integrated with a member’s full benefit ecosystem, virtual care teams can also guide patients to appropriate in-person care when it’s needed.
The cost savings from VPC can extend beyond direct replacement costs, however. Another layer of value provided by VPC is indirect savings. Employers often deploy various benefit and workplace strategies to maintain the health and presence of their workforce. Virtual primary care can indirectly contribute to further savings by keeping members healthy and reducing absenteeism.
As an example, a nationwide employer leaned into VPC and implemented a program where they saw an 11% reduction in the total cost of care among employees who accessed VPC. Additionally, hospital readmissions among their VPC members decreased by an impressive 26%, while inpatient hospital costs saw a substantial 38% reduction. Moreover, after utilizing VPC, only approximately 10% of members sought in-person care within 21 days, meaningfully reducing other low-value and unnecessary care.
Our virtual primary care solution offers a comprehensive approach, allowing members access to both medical and mental health care. Numerous studies have highlighted the substantial value and savings resulting from coordinated care between medical and behavioral health services. This integration not only enhances the overall healthcare experience, but it also leads to considerable savings.
These findings challenge the common belief that virtual primary care is merely an “additional expense” without a proven return on investment (ROI), leading to costly overuse. On the contrary, the data underscores that prioritizing primary care not only enhances member well-being, but it also serves as a strategic move to contain healthcare expenses on a broader scale.
For a leading employer, virtual primary care delivered
Myth #2:
Virtual primary care is only used by the young and healthy
Virtual primary care is not just used by millennials and Generation Z. In a multi-state pilot program of more than 350,000 covered lives, a nationwide employer saw that a third of the adult members who used virtual care were 45 or older. This aligns with Included Health’s data where >27% of our VPC members fell into the 45 or older age group, highlighting the broad appeal and accessibility of VPC across various age demographics.
Reality #2:
VPC is utilized across age groups and addresses diverse healthcare needs
And VPC is not just about treating “simple sick” issues. In reality, it’s proven to be a versatile solution for addressing the full spectrum of healthcare needs. Across our entire population, we’ve seen that 30% of members sought virtual care for chronic conditions or preventive care, demonstrating its effectiveness in managing and preventing long-term health issues. This becomes even more significant when you consider that 82% of Included Health members who utilized VPC had not seen an in-person primary care provider prior to their first virtual visit.

1 in 3
adults who used virtual care were 45 or older
Even more interestingly, the employer found that 37% of members who had a VPC visit also utilized the service for virtual mental health support like therapy and psychiatry, underscoring the reality that patients desire a care setting that can support their whole health—both mental and physical. When primary care providers are cross-trained to support behavioral health, they can truly deliver whole-person care, acting as the front line to detect and guide members to the right care resources. Additionally, through true practice integration, Included Health members have access to a full behavioral health practice that treats 50+ conditions.
And similarly in brick and mortar settings, VPC is not just a one-and-done deal. A substantial 40% of adults in the study with three or more acute visits eventually returned for ongoing management of a chronic condition. This further dispels the myth that virtual care only offers quick fixes. It’s a dynamic care setting that can accommodate a wide range of healthcare needs, regardless of age or the complexity of the healthcare condition, and can foster long-term relationships between patient and provider for ongoing care needs.
Our care team delivers:
Clinical Care, including Chronic Care Management
- Hands-on support
- Condition education
- Prevention
- Care planning
- Medication therapy management
- Nutrition support
Care Coordination Support
- Assistance with social determinants of health concerns
- Coordination between provider visits
- Follow-up for all VPC Members, from low to high risk
Myth #3:
Only in-person visits can deliver high-quality care
In the ongoing discussion on virtual healthcare, a common assumption is that virtual care falls short in delivering high-quality care when compared to in-person office visits.
Reality #3:
VPC breaks down access barriers by providing care where and when individuals need it
Virtual primary care isn’t just a viable alternative for traditional in-person visits. Recent data trends, obtained from both a nationwide employer study and Included Health’s proprietary data, underscore its capacity to deliver better health outcomes.
Noteworthy progress from the employer pilot was observed in healthcare outcomes:
Diabetes management saw a significant improvement, with a 24% reduction in HbA1c levels.
High blood pressure showed positive progress as well, with a 14% reduction (matching the 15% reduction observed among all Included Health members).
Mental health support had a remarkable impact, with a 40% reduction in PHQ-9 scores among members treated for depression (across all Included Health members the numbers are even more exciting, experiencing a 56% reduction when incorporating therapy and psychiatry services).

What makes these achievements even more powerful is that they extend beyond demographic boundaries. This progress is consistent across various communities, including those residing in rural areas, low-income households, and Black and Hispanic communities. It's evidence that virtual primary care can effectively break down access barriers, provide individuals the care they need, when they need it, and help ensure healthcare access for all.
Furthermore, it's crucial to recognize that the choice between virtual and in-person care shouldn't be an either/or decision. While in-person visits have long been the gold standard in healthcare, recent advancements in technology and healthcare delivery models have transformed the landscape. Virtual healthcare, once perceived as a stopgap, is now proving to be a reliable and effective means of providing quality care. It offers a host of benefits, including convenience, accessibility, and the ability to reach underserved populations. Moreover, data trends reveal that virtual care can not only match but also exceed the quality of in-person care, particularly when it comes to managing chronic conditions and providing mental health support. In the ever-evolving healthcare landscape, it's crucial to embrace this promising blend of technology and medicine and recognize the potential it holds for delivering high-quality care to a broader and more diverse patient population.
The choice between virtual and in-person care shouldn't be an either/or decision.
Conclusion
Dispelling myths about virtual primary care is essential to understanding its potential in modern healthcare. VPC allows providers to break free from the constraints of location and deliver comprehensive, quality care that meets members where they are. Investing in virtual primary care isn't just a smart financial decision. It's a commitment to better health and a strategy to avoid unnecessary costs on a larger scale. The data is clear: VPC is not an unattainable vision or “just another expense.” It’s a proven, turnkey solution that paves the way for a more accessible, efficient, and comprehensive healthcare experience for everyone.