All-Included Care™ is an integrated healthcare platform that combines clinical navigation, virtual care, and benefits advocacy into a single, connected experience. Unlike traditional point solutions, All-Included Care unifies medical, behavioral, and specialty care with one app, one team, and one data source—helping employers reduce costs while improving employee health outcomes.

Real healthcare integration, real results
>4%
Y1 reduction in healthcare trend across our BOB
+2
Healthy Days per month for clinically-engaged members
~80%
annual household engagement
$2,000
avg. savings for clinically-engaged members
>80%
of behavioral health-engaged members see improved mental health
Addressing health needs across your full population
Proud to work with leading organizations


Why it works



Discover the value of integrated healthcare
We’re amplifying impact with AI+EQ
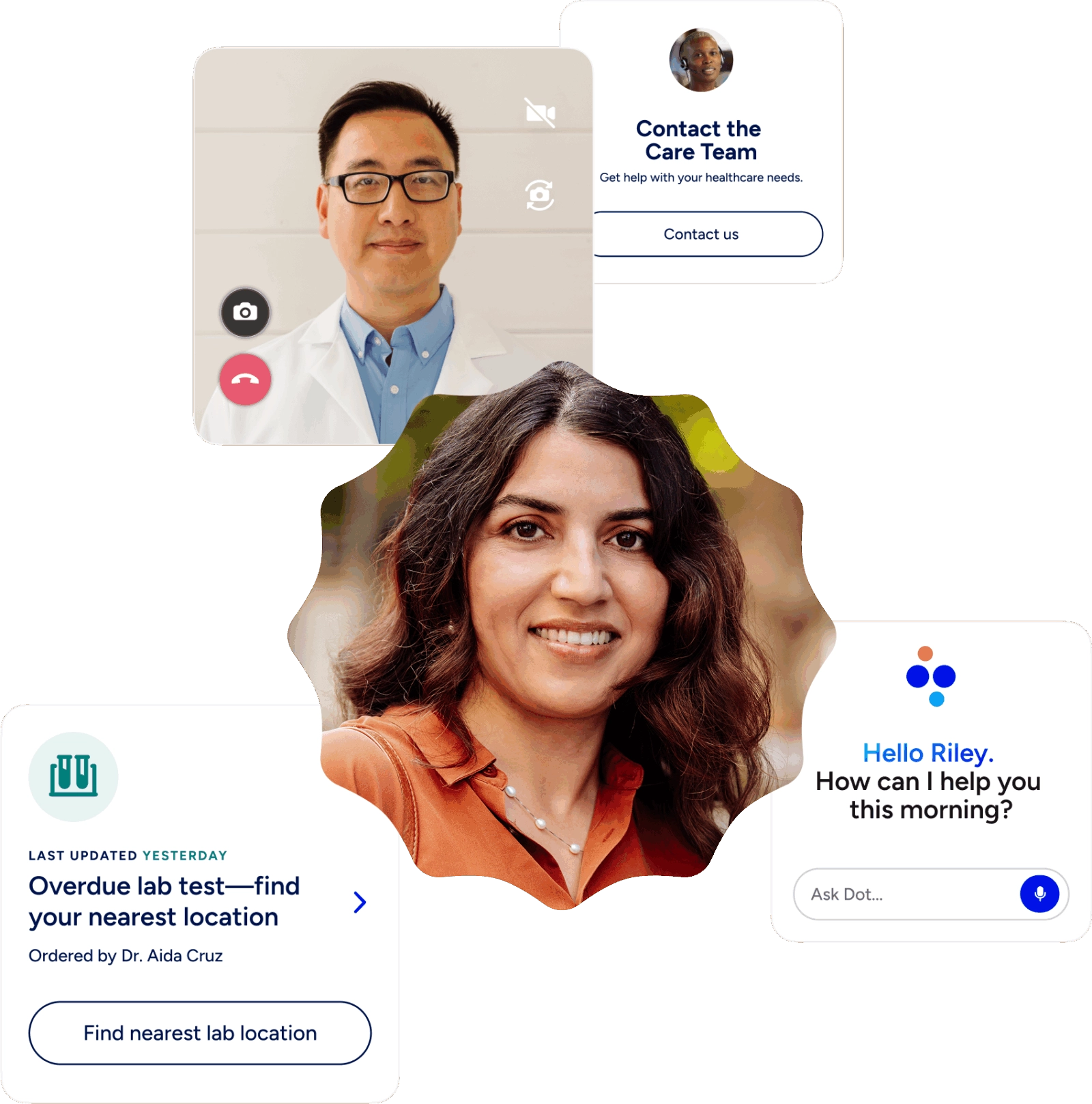
At Included Health, we believe the future of healthcare isn't just about technology, it's about people. Our unique AI+EQ approach combines powerful artificial intelligence with genuine emotional intelligence to rehumanize healthcare.
We use smart, safe technology to enhance, not replace, the invaluable human touch, ensuring every interaction is personalized, empathetic, and effective.
The Included Health difference
-
All-Included Care™
Others
-
Model
Integrated, virtual-first care with in-house clinical teams and data-driven insights. All services are available in one app to create a seamless experience.
Fragmented, disjointed solutions that bolt together separate services, leading to a confusing and low-quality experience.
-
Personalization & technology
Human-centric AI that augments products and empowers clinical and advocacy teams to provide truly personalized care. AI tools like Provider Match and our generative AI digital agent, Dot, enhance a fully integrated platform.
AI used as a "bandaid" or a replacement for human help. Technology may not be fully integrated, leading to a lack of clinical depth.
-
Data & integration
Seamlessly connected data from medical claims, pharmacy, cost, quality metrics, and social data. This is leveraged through a certified Electronic Health Record (EHR) that supports coordinated care across multiple providers.
Siloed data sources that make it difficult for providers to get a holistic view of a patient's health. The lack of integration creates logistical barriers and a disjointed experience.
-
Services & support
Core services in one place, that include care delivery, benefits guidance, claims advocacy, and 24/7 answers to healthcare questions. This simplifies the experience and centralizes accountability with a single partner.
Overwhelming number of point solutions for specific conditions. This complicates navigation for both employers and employees, and hampers opportunities to engage people across their full healthcare journey.
-
Partnership & accountability
Innovative partnership model with aligned incentives. Shared risk and reward, total population health commitments, and aggressive trend targets ensure a long-term, sustainable partnership focused on meaningful outcomes and cost reduction.
Fee-for-service models that don’t align incentives. Some models steer patients to narrow networks and lack the strategic partnership needed to drive long-term value.
-
Value
Proven ROI and trend reduction. The integrated approach drives outcomes that matter to employees and the business, leading to increased productivity and talent retention.
Commitments to high engagement or cost savings without the quality-driven guidance or clinical expertise needed to deliver longitudinal impact.
96%
Primary Care provider satisfaction rating
<10 min
wait time for on-demand care
↑77%
of members experienced improved blood pressure
↓24%
Reduction in HbA1c levels among members with diabetes








