
Included Health shows a significant reduction in symptoms of depression with virtual mental health care
Better access, better care for every mental health need
One in five Americans experience a mental illness each year. Effective behavioral health treatment can help people overcome mental illness, improving health and changing lives. To measure the efficacy of Included Health behavioral health treatment, the company analyzed patient PHQ-9 scores, reflecting the severity of depression symptoms, in a subset of patients with diagnosed depression. Preliminary results found significant improvements in PHQ-9 scores for patients over a course of treatment with a psychologist or psychiatrist, exceeding industry benchmark outcomes for in-person treatment.
For patients with four psychiatry visits, over 60% were able to improve PHQ-9 by at least 50% and reduce PHQ-9 below 10. For patients with eight behavioral therapy treatments, 44% of patients were able to improve PHQ-9 by at least 50%, and 55% of patients achieved a PHQ-9 below 10. These findings demonstrate that virtual mental health care is an effective clinical approach to reduce the symptoms of depression.
Background
An estimated 17 million Americans—7% of the population—had a major depressive episode in the past year. More than 20% of American adults experience mental illness each year. Yet, less than half of those suffering receive treatment. The cost of untreated mental illness is detrimental for patients, employers, and the healthcare system. Individuals with mental illness have significantly higher medical costs and a greater risk of developing chronic disease. Without treatment, patients experience lower levels of productivity, performance at work, and overall quality of life.
It is vital that patients who experience mental illness receive effective treatment. However, there are vast barriers to access for many Americans. On average, it takes 25 days for a new patient to see a psychiatrist in some of the largest U.S. cities. Many geographic areas have little to no access to psychiatrists at all. More than 60% of U.S. counties do not have a psychiatrist, and rural counties only have 590 total psychiatrists to serve more than 27 million Americans.
Availability and ease of access is not only an initial barrier to treatment, but also a factor in treatment outcomes. The odds of response and remission to psychiatric care decrease by 9% for every week in between the first consultation and follow-up. High costs of care and stigma related to seeking care add additional obstacles to treatment.
As a virtual care provider, Included Health connects patients to licensed therapists and psychiatrists via video to overcome barriers and improve patient mental health. Its nationwide practice of providers supports patients with a range of services including behavioral therapy and medication management. Through its secure, HIPAA-compliant technology platform, patients receive care at any time, from any location, across all 50 states, 7 days a week. On average, Included Health patients only wait 1-5 days to see their mental health provider, and less than 10 minutes to see a physician for immediate behavioral health intervention. The rapid availability of initial consultation appointments is significant for those with acute concerns or those in crisis, and follow-up appointment availability ensures consistent treatment. Insurance is not required to access Included Health, but appointment costs are covered in full or part for millions of Americans through their health plan or employer.
Mental illness in the U.S.
About the study
To measure the efficacy of its virtual behavioral health program, Included Health analyzed outcomes for patients with a clinical depression diagnosis. The study focused on patients with depression due to the prevalence of the condition in the general population and the established data from symptom severity assessments.
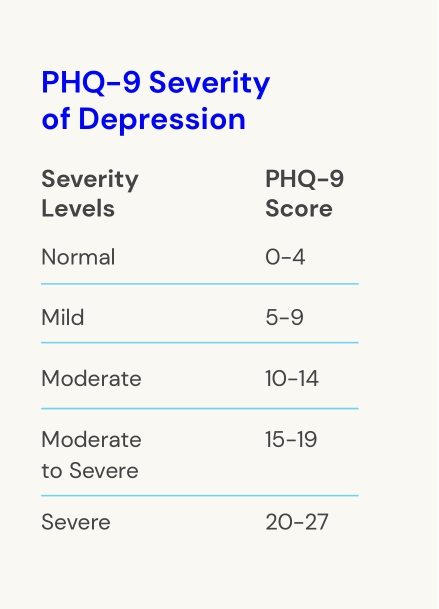
The Patient Health Questionnaire (PHQ-9) measures severity of depression and can be administered repeatedly. The efficacy and reliability of the PHQ-9 score to measure depression is widely established, and the assessment has been broadly adopted by mental health professionals. Included Health uses the PHQ-9 both as a screening tool and during the course of behavioral health treatment to diagnose, guide treatment, and measure patient progress. PHQ-9 scores range from 0 to 27; scores under 5 are normal; scores of 5 to 9 indicate mild depression; scores of 10 to 14 indicate depression of moderate severity; and scores of 15 and higher indicate depression that is moderately severe to severe.
Included Health administers the PHQ-9 prior to each mental health visit throughout the course of a patient’s treatment. The company’s data team analyzed the change in PHQ-9 scores for a subset of patients who received virtual behavioral health care between July 2019 and February 2020. Patients were included in the study if their initial PHQ-9 score was greater than or equal to 10, they had at least two PHQ-9 scores, and they registered and received treatment within the study date range. In total, 2,320 patients were included in the study. The initial and most recent PHQ-9 score for each patient was compared and results were evaluated in sub-groups based on length of course of treatment and modality of treatment.
Better mental health treatment outcomes
Psychiatry
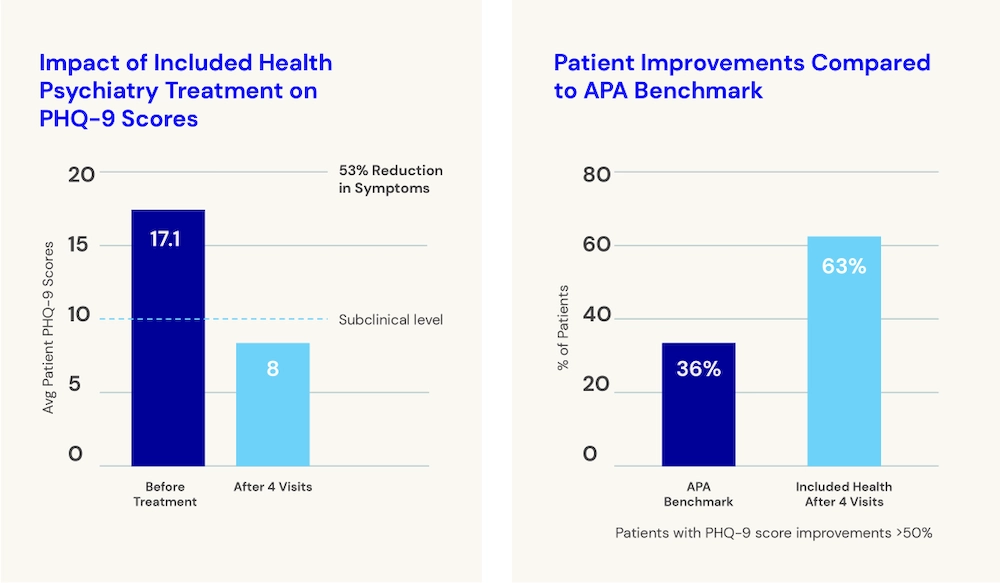
For psychiatry, Included Health outcomes were evaluated for a 4-visit course of treatment. Over 40% of patients achieved full remission (PHQ-9 < 5) in four visits. The average PHQ-9 score improved by 53%, moving from 17.1 to 8.0, a score in the mild range. More than 60% of patients were able to improve PHQ-9 by at least 50% and reduce PHQ-9 below 10. Patients with a PHQ-9 score of less than 10 would experience either mild or no symptoms. They would be expected to experience less daily distress, see increased productivity, improved relationships, and a significantly improved quality of life as compared to patients in the moderate to severe clinical ranges.
The American Psychiatric Association’s (APA) industry benchmark for in-person depression treatment is a remission rate of 18% over a 24-week period. In the APA study, 36% of patients’ PHQ-9 scores improved by at least 50% compared to 63% of Included Health patients. Additionally, in the APA study, 45% of patients’ PHQ-9 scores were lowered to less than 10 compared to 66% of Included Health patients.
Reduction in symptoms
Behavioral therapy
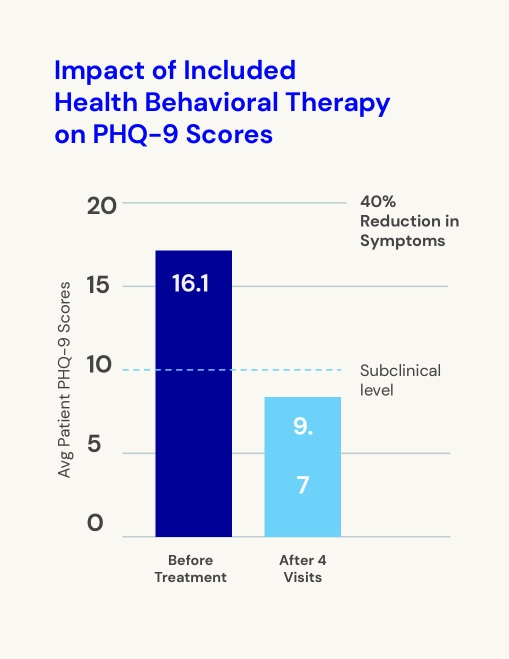
For behavioral therapy, the standard course of treatment is longer than psychiatry, generally 6-8 visits. With eight Included Health appointments, 42% of patients achieved full remission (PHQ-9 < 5). The average PHQ-9 score improved by almost 40%, from 16.1 to 9.7, representing a final score in the mild symptom range. Average final score was driven by symptom improvements across the patients in the study; 44% of patients were able to improve PHQ-9 by at least 50%, and 55% of patients achieved a PHQ-9 below 10, experiencing mild or no symptoms.
65% of Included Health patients showed an improvement of at least 25% in PHQ-9 score in eight visits. For comparison, American Psychology Association benchmarks predict only 50% of patients achieve a measurable improvement in symptoms after eight visits.
Reduction in symptoms
The value of virtual behavioral health
Virtual behavioral health care that puts patients face-to-face with a mental health provider in a video visit is highly effective for treating depression, exceeding APA benchmarks for in-person treatment. In this study, Included Health demonstrated positive outcomes for patients by measuring PHQ-9 scores in both psychiatric and psychological treatment settings.
These results come as consumers report a growing interest in receiving more types of health care virtually. Delivering care virtually removes traditional barriers and can exponentially increase the number of Americans who can access and benefit from mental health services. Included Health expands nationwide patient access to high-quality behavioral health care with licensed therapists and psychiatrists. Providers are consistently available and accessible for talk therapy, medication management, and frequent follow-ups.