Pre-deductible coverage and receipt of telemental health visits
Study motivation
The marked increase in telehealth visits, particularly for mental health, during the COVID-19 pandemic was bolstered by regulatory changes such as the exemption of telehealth visits from the deductible in high-deductible health plans in which individuals face a minimum $1600 deductible. Congress extended this exemption through the end of 2024, and there is ongoing debate on whether the exemption should be made permanent. Given that there has been no empirical data on the effect of this exemption, we collaborated with researchers from Harvard Medical School and the University of Michigan to examine utilization changes associated with the reintroduction of cost sharing for patients receiving telemental health.
Methodology
- Cohort study with patients from all 50 states and the District of Columbia receiving telemental health care from Included Health from two clients that varied in their coverage of telemental health during the study period
- During the pre-intervention period (January 1 to June 30, 2021), all patients had no cost sharing for telehealth visits
- In July 2021, one client (intervention) reintroduced cost sharing, and the other client (control) continued to offer telehealth services without cost sharing
- We used difference-in-difference methodology to evaluate how the reintroduction of cost sharing was associated with telehealth use in the post-intervention period (July 1 to December 31, 2021)

What we found
- In the 6-month pre-intervention period, the intervention and control groups had a mean of 4.8 and 4.7 telemental health visits per patient, respectively
- After reintroduction of cost sharing in the intervention group, the mean number of visits per patient per month was lower in the intervention group than the control group
- For the intervention group, cost sharing was associated with 1.5 fewer visits per patient and an 11.7% reduction in the proportion of patients who had any visits in the post-intervention period
Average number of telemental health visits per patient by cohort before and after cost sharing was introduced in the intervention group*
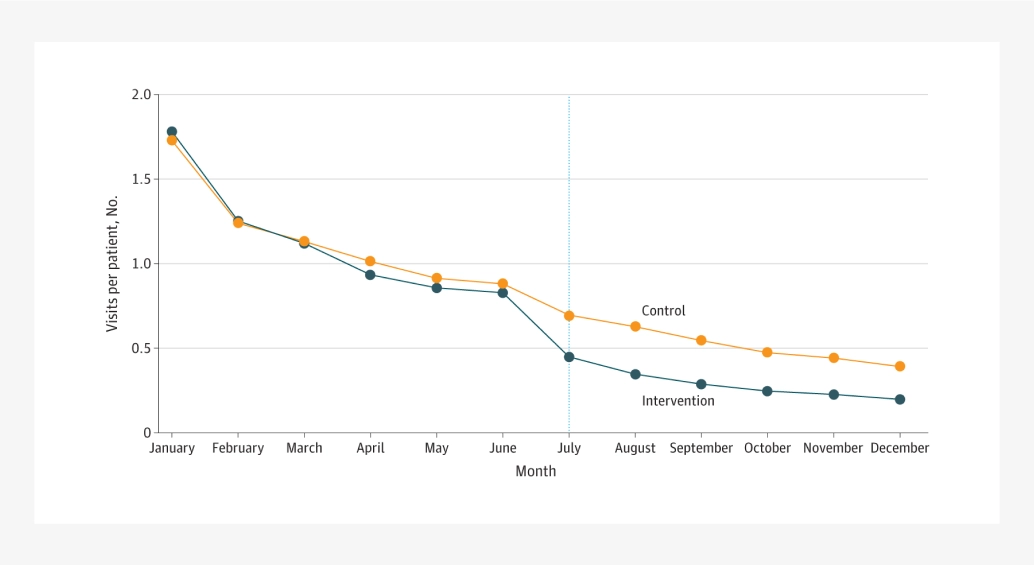
*Vertical blue dotted line indicates when cost sharing was introduced in the intervention group
Implications
- We found that when patients were required to pay out of pocket for telehealth visits, they had substantially fewer telemental health visits, and a larger fraction stopped seeing their mental health specialists
- These findings imply that the expiration of the pre-deductible telehealth coverage exception in January 2025 may reduce mental health service use, which could lead to worse clinical outcomes
- Given ongoing concerns about access to mental health treatment and to help patients stay in treatment, policies that reduce cost sharing for both in-person and telemental health visits should be considered
Fang K, Marshall J, Fendrick AM, Huskamp HA, Thomas L, Mehrotra A. Predeductible Coverage and Receipt of Telemental Health Visits. JAMA Netw Open. 2024;7(7):e2420731. doi:10.1001/jamanetworkopen.2024.20731.
Author affiliations:
Kacey Fang, Department of Health Care Policy, Harvard Medical School
Jaclyn Marshall, Department of Health Economics and Outcomes Research, Included Health
A. Mark Fendrick, Center for Value-Based Insurance Design, University of Michigan
Haiden Huskamp, Department of Health Care Policy, Harvard Medical School
Latoya Thomas, Department of Policy and Government Affairs, Included Health, Washington, DC
Ateev Mehrotra, Department of Health Care Policy, Harvard Medical School; Division of General Internal Medicine Beth Israel Deaconess Medical Center