Healthcare AI has to deliver more than efficiency
AI will fail to improve outcomes and reduce costs if we don't put it to work for people.

AI is showing once again that old habits in healthcare die hard. The AI revolution has created a once-in-a-generation opportunity to transform how people access and experience care, but so far the technology has been deployed in mostly predictable and less-than-transformative ways.
Consider providers and payers. Both are racing to build AI into their respective businesses, and both claim to be using the technology to improve the healthcare experience. Yet their collective investments in AI are heavily skewed toward boosting their own bottom line, which we know doesn't always benefit their patients and members (respectively).
In a recent McKinsey report on generative AI, health systems and payers both identified administrative efficiency and clinical productivity as the top areas of value for their organization. Patient and member engagement and quality of care lagged well behind on the list.
These priorities speak volumes about the state of the U.S. healthcare system, and point to a much bigger problem than lack of efficiency: lack of trust.
Patients and members — or as I like to call them, "people" — figured out a long time ago that the system isn't designed to work for them. Access barriers, confusing coverage, disappointing doctors' appointments, surprise bills, and the overall frustration and fragmentation of the healthcare experience have led them to give up and disengage. Too often, that means delaying or avoiding essential care until preventable issues turn into costly ER visits and hospital stays.
Engagement, not efficiency, is the key to reversing deteriorating outcomes and escalating system-wide costs. Yes, AI can help providers and payers with admin burden and cumbersome workflows, but that's not where real transformation will be found. AI will only move the needle on outcomes and costs when we put it to work for people.
New technology, same-old story
Providers and payers have been giving their patient portals and digital front doors an AI facelift, but the experience remains largely unchanged. In fact, engagement and experience represents a fraction of their AI investment.
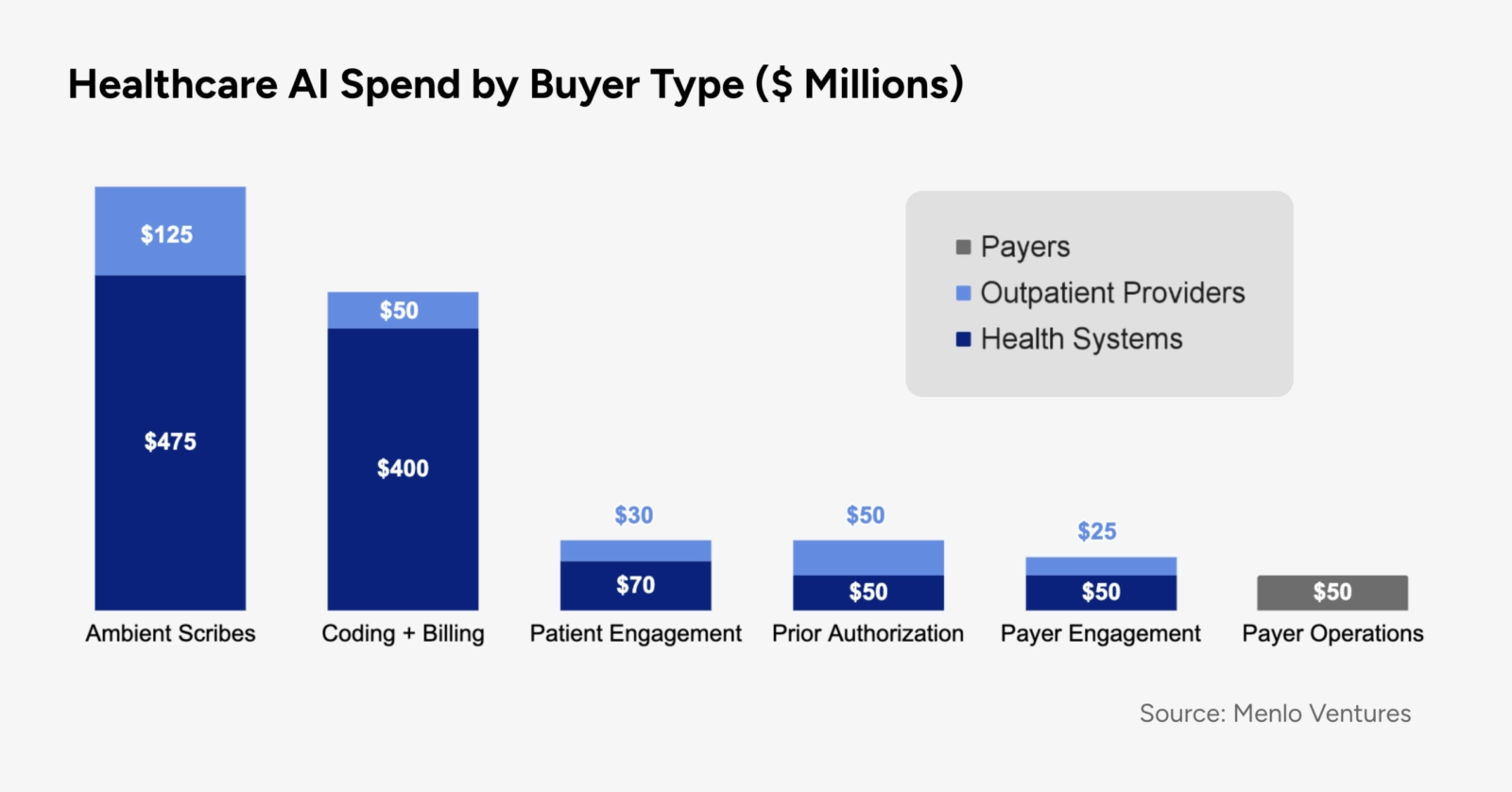
On the provider side, the focus instead is on capabilities such as ambient scribing and automated coding and billing that deliver quick "time to value" by reducing staffing and improving revenue cycle management. On the payer side, top AI use cases include fraud detection, utilization management, and risk adjustment — functions not known for being especially member-friendly.
What's more, providers and payers are increasingly mobilizing AI investments against each other in the eternal fee-for-service Cold War. One high-profile example: Physicians and hospitals, alarmed by an apparent AI-driven increase in denied claims, are building up an arsenal of AI tools to automate and bolster appeals.
AI technology might be game-changing, but only if the game itself changes. In a promising development, innovators outside the traditional payer-provider orbit are thinking bigger than reimbursement and coding, and are using AI to create a new healthcare experience that delivers value to people and healthcare purchasers alike.
A modern healthcare experience
Healthcare chatbots designed to streamline symptom checking, patient triage, coverage questions, and myriad other healthcare interactions are already ubiquitous. While these bots have definitely made certain tasks faster, they're also trapped in the same-old silos.
Speed and convenience aren't enough; people also care about continuity, quality, and relationships. They don't want to interact with 10 different bots. They want a single, personalized experience that supports the full range of their clinical, financial, and administrative needs and that makes them feel seen, heard, and understood across the entire system.
That experience is finally a reality, but it requires more than just chatbots. It requires purpose-built AI assistants that are connected to the full stack of data, systems, and resources that underpin the healthcare experience, including medical and pharmacy claims, benefits and coverage info, physician quality data, and — most importantly — empathetic human care teams. This, not automated billing, is the intelligent back-end innovation necessary to restore trust and deliver value.
When people engage in this comprehensive and highly personalized experience, it creates opportunities for AI and human clinicians to identify gaps in care, proactively surface recommendations and next steps, follow up after doctor's appointments, and more — always with the option to hand off to human experts when needed. Over time, this experience builds trust, and trust drives repeat engagement, one of the strongest levers for improving health outcomes and lowering costs.
Who is AI for?
Of course the healthcare system is inefficient. Harnessing AI to address provider burnout, outdated systems, and waste are all worthwhile objectives. But they're not exactly inspiring, and the technology is capable of so much more.
As new uses for AI emerge, everyone working in healthcare should be asking some fundamental questions. Who is this technology actually serving? Is it making high-quality care more accessible for everyone? Is it reducing costs for households and businesses? Is it bringing us closer to the healthcare experience we all want for ourselves and our loved ones?
Or is it helping the existing system work against us more efficiently?

Nupur Srivastava, SVP of Product
About the author
Nupur Srivastava is Included Health’s chief operating officer. She leads the care team, as well as engineering, product, design, data, and information technology.

